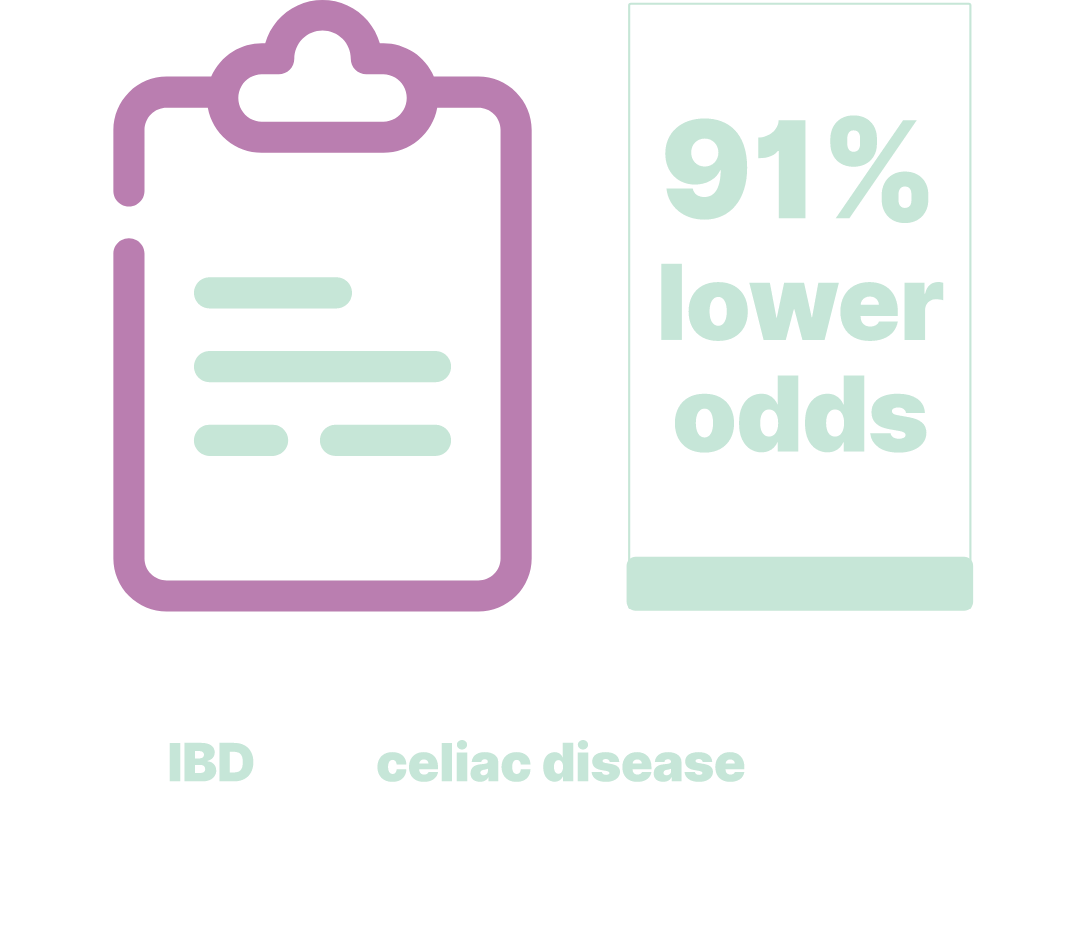
A survey used phone interviews with Black (n=137) and White (n=149) patients with IBD from 2005 to 2008.
aAfter adjusting for age, age at diagnosis, sex, comorbidity, health insurance payer, educational attainment, income, and prolonged steroid use3
Limitations: The patient population was from a tertiary medical center, which often includes more patients with chronic steroid use and more-severe illness than would be observed in a community setting. Health utilization data were based on patients self-reporting. Medical records used in the study might not provide a comprehensive assessment of healthcare utilization; most patients received care at additional healthcare institutions. Patients in this study may not represent the larger IBD patient population.3